Is the End of Private Psychotherapy Practice in Sight?
The current environment of Healthcare is dominated by venture capital investors. As a result, psychotherapist must rethink how psychotherapy is going to be marketed and delivered. But can a profession of individual practices reach the same conclusions and invest resources during a pandemic in their collective future. Change may be difficult because private psychotherapy practice is focused on one patient at a time, not public health.
New terminology is required if private practice is going to survive and thrive. A “gig economy” is a labor market characterized by the prevalence of short-term contracts or freelance work as opposed to permanent jobs. That is how private practice works. When the demand for services is high and supply of therapists is low, venture capital companies thrive.
According to Ryan Schwartz (Founder of Mental Health Match, the “gig economy” is not a good fit for therapy, despite how much venture capitalists try to force the model on the profession. There are better solutions to the challenges that exist for therapists and clients, but those solutions need action and support if private practice therapists going to have chance to survive in the new landscape of mental health care.
Healthplans historically focus on increasing profits by utlization review practices that restrict care often based hidden medical necessity criteria that is ill-defined. Healthplans now want data that can be used to compare providers to each other and thereby limit services to those that are medically necessary in some objective way that is not based on a therapist clinical opinion. To do that, Healthplans are using venture capital managed start-up companies.
Venture capital start-ups want:
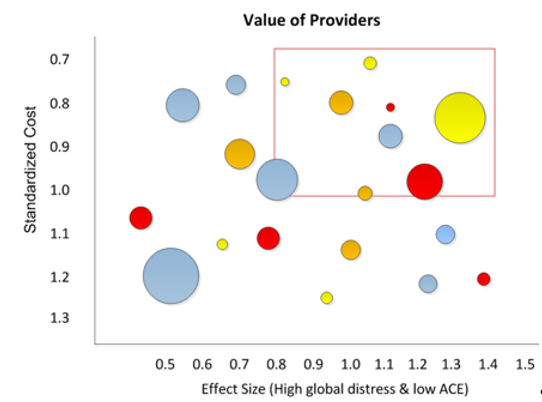
In the above image, the provider in the upper right corner are measurably the most effective and valuable providers
psychotherapists to contract with them (drop their existing contract),
psychotherapists to use their online calendar to schedule appointments,
to administer online electronic progress and satisfaction questionnaires on behalf of psychotherapists, and
to manage provider services in ways that save millions of dollars in healthcare costs.
To make venture capital companies successful, psychotherapists must allow the start-up to administer questionnaires to patients. The latter allows the start-up to use that data and to sell that data and information to the Healthplan. Unfortunately, giving that data away allows a Healthplan monetize the data psychotherapists could have monetized. With the data gathered, Healthplans can identify the providers they consider effective and those who are not. Not surprisingly, Healthplans are encouraging and financially supporting electronic outcome measurement systems that target symptom burden and functional problems.
For more information see:
Do Venture-Capital Investors Think Psychotherapists are Dumb?
www.amha-or.com/are-psychotherapists-dumb
Ryan Schwartz (Founder of Mental Health Match), wrote,
New tech companies with a lot of money are shaking up the therapy industry in a way that is threatening the independence of psychotherapists and their ability to offer high-quality, effective mental health care.
Since the pandemic began, more people have started paying attention to their emotional and psychological wellbeing. So, too, have venture capitalists. In 2020, investors spent $2.4 billion to buy and build mental health companies. Much of that money is fueling a shift in how therapists provide therapy and get paid.
These companies profit by amassing huge networks of contracted therapists and providing access to those contractors. It’s the same “gig economy” model that gave rise to Uber, but applied to therapists and their clients. In startup speak, these companies are “disrupting” the traditional private practice model of providing care in the same way Uber “disrupted” the private taxi industry.
The problem is that therapeutic healing is not a transaction or commodity; it’s a relationship that must be nurtured. The effectiveness of therapy depends on the strength of that relationship.
For more information see:
Is the End of Private Psychotherapy Practice in Sight?
https://mentalhealthmatch.com/articles/for-therapists/end-private-practice-therapist
According to Cerebral, the largest venture capital backed online behavioral health company in the U.S….
…access to care remains a major barrier. Patients wait months before they can access care, and when they do, the quality of care is poor. The vast majority of mental health clinicians do not systematically monitor clinical outcomes, which hinders efforts to understand the impact of their clinical interventions .
Clinical data is underused in mental health despite conclusive research demonstrating that thoughtful use of patient-reported outcomes can improve quality . Furthermore, research suggests that improving access to mental healthcare can improve employees’ well being and increase job satisfaction.
Cerebrals has raised 1.4 billion dollars and has a recent “valuation” of 4.6 billion dollars. Cerebral has the money, technology, methods and ambition to manage every aspect of psychotherapy practice. The associated cost for services are:
Medication and Therapy: $325 per month. The first month is $139 .
Medication and Care Counseling: $85 per month. The first month is $30 .
Therapy: $259 per month. The first month is $99.
New online services (e.g. Teledoc, Zoom) have surfaced in recent years. Still, the overall patient experience remains confusing and disorganized while patients are downloading a smartphone app for mindfulness, signing up for a therapy service, and registering for yet another service for medication prescriptions and management. This fragmented approach is not only inconvenient, but it also compromises quality given that the clinicians on these separate services do not coordinate care. In the current state of affairs, patients, provider, payers and Healthplans lose out. Employers and payers spend more on ineffective and uncoordinated care, clinicians are not empowered to practice high quality services. Patients suffer.
The pandemic is forcing psychotherapists to rethink their relationship with mental health and healthcare in general. Telehealth has become mainstream, and there is increasing recognition that this mode of delivering outpatient care could be as effective as in-person care. In addition to convenience, telehealth affords patients the privacy of seeking care without having to visit a clinic. Social stigma remains a major barrier for those considering mental healthcare, and telehealth models suggest that they improve care and especially preventative care. But there is doubt among psychotherapist that the research on equivalency is not substantial and cannot be generalized to entire populations.
Finally, organizations are becoming increasingly aware of how mental health affects total healthcare spend and worker productivity. Every dollar invested in mental health can result in as much as $7 of increased productivity and savings in medicial costs.
References
Author, (2013) Patient Reported Outcomes (PROs) in Performance Measurement. National Quality Forum. http://www.qualityforum.org/publications/2012/12/patient-reported_outcomes_final_report.aspx
Author, Turning Point Clinically Informed Outcomes. http://www.turningpointfoundation.org/ways-to-care/resources/
Barry, M. M., Clarke, A. M., Petersen, I., & Jenkins, R. (Eds.). (2019). Implementing mental health promotion. Springer Nature.
Bashshur, R. L., Shannon, G. W., Bashshur, N., & Yellowlees, P. M. (2016). The Empirical Evidence for Telemedicine Interventions in Mental Disorders. Telemedicine journal and e-health : the official journal of the American Telemedicine Association, 22(2), 87–113. https://doi.org/10.1089/tmj.2015.0206
Brown, G.S., Simon, A., Cameron, J., & Minami, T. (2015). A collaborative outcome resource network (ACORN): Tools for increasing the value of psychotherapy. Psychotherapy, 52:4, 412-421. https://pubmed.ncbi.nlm.nih.gov/26641371/
Bubonya, M., Cobb-Clark, D. A., & Wooden, M. (2017). Mental health and productivity at work: Does what you do matter?. Labour economics, 46, 150-165. https://www.sciencedirect.com/science/article/abs/pii/S0927537116301506
Burton, W. N., Schultz, A. B., Chen, C. Y., & Edington, D. W. (2008). The association of worker productivity and mental health: a review of the literature. International Journal of Workplace Health Management. https://www.researchgate.net/publication/244906193_The_association_of_worker_productivity_and_mental_health_A_review_of_the_literature
Chisholm, D., Sweeny, K., Sheehan, P., Rasmussen, B., Smit, F., Cuijpers, P., & Saxena, S. (2016). Scaling-up treatment of depression and anxiety: a global return on investment analysis. The Lancet Psychiatry, 3(5), 415-424.
Collaborative care for patients with depression and chronic illnesses. The New England journal of medicine, 363(27), 2611–2620. https://doi.org/10.1056/NEJMoa1003955
Dandachi, D., Dang, B. N., Lucari, B., Teti, M., & Giordano, T. P. (2020). Exploring the attitude of patients with HIV about using telehealth for HIV care. AIDS patient care and STDs, 34(4), 166-172.
Duncan, B.L., & Reese, R.J., (2015). The partners for Change Outcome Management System (PCOMS): Revisiting the client’s frame of reference. Psychotherapy, 52:4, 391-401. https://pubmed.ncbi.nlm.nih.gov/26641369/
Gilbody, S. M., House, A. O., & Sheldon, T. A. (2002). Outcomes research in mental health: Systematic review. The British Journal of Psychiatry, 181(1), 8-16. https://www.cambridge.org/core/services/aop-cambridge-core/content/view/7BE531EF71A88E95106AB27B087362E2/S000712500016146Xa.pdf/div-class-title-outcomes-research-in-mental-health-div.pdf
Guo, T, et al (2015) Measurement-based care versus standard care for major depression: A randomized control trial with blind raters. American Journal of Psychiatry, 172:10, 1004-1013. https://pubmed.ncbi.nlm.nih.gov/26315978/
Heaney, C. A., Price, R. H., & Rafferty, J. (1995). Increasing coping resources at work: A field experiment to increase social support, improve work team functioning, and enhance employee mental health. Journal of organizational behavior, 16(4), 335-352 .
Howard, K., Kopta, SM., Krause, MS., and Orlinsku, DE (1986). “The Dose-Effect Relationship in Psychotherapy.” American Psychologists 41:2; 181-187. https://i-cbt.org.ua/wp-content/uploads/2017/11/Howard-dose_effect-psychotherapy-1986.pdf
Irvine, A., Drew, P., Bower, P., Brooks, H., Gellatly, J., Armitage, C. J., ... & Bee, P. (2020). Are there interactional differences between telephone and face-to-face psychological therapy? A systematic review of comparative studies. Journal of Affective Disorders, 265, 120-131.
Kadera, SW, Lambert, MJ, and Andrews, AA “How Much Therapy is Really Enough?” (1996) Journal of Psychotherapy Practice and Research. https://pubmed.ncbi.nlm.nih.gov/22700273/
Katon, W. J., Lin, E. H., Von Korff, M., Ciechanowski, P., Ludman, E. J., Young, B., Peterson, D., Rutter, C. M., McGregor, M., & McCulloch, D. (2010).
Kilbourne, A. M., Beck, K., Spaeth‐Rublee, B., Ramanuj, P., O’Brien, R. W., Tomoyasu, N., & Pincus, H. A. (2018). Measuring and improving the quality of mental health care: a global perspective. World psychiatry, 17(1), 30-38.
Kopta, M., Owen, J., & Budge, S. (2015). Measuring psychotherapy outcomes with the behavioral health measure-20: Efficient and comprehensive. Psychotherapy, 52:4, 442-448. https://pubmed.ncbi.nlm.nih.gov/26315978/
Lambert, M.J. (2015). Progress feedback and the OQ-System: The past and the future. Psychotherapy, 52, 381-390. https://pubmed.ncbi.nlm.nih.gov/26641368/
Lewis, C. C, Scott, K., Marti, C.N., Marriott, B.R., Kroenke, K., Putz, J.W., Mendel, P., & Rutkowski (2015). Implementing measurement-based care (iMBC) for depression in community mental health: A dynamic cluster randomized trial study protocol. Implementation Science, 10:127. https://pubmed.ncbi.nlm.nih.gov/30566197/
Lewis, C.L., Boyd, M., Puspitasari, A., Navarro, E., Howard J., Kassab, H., Hoffman, M., Scott, K., Lyon, A., Douglas, S., Simon, G., Kroenke, K. (2018) Implementing Measurement-Based Care in Behavioral Health: A Review, doi:10.1001/jamapsychiatry.2018.3329 https://pubmed.ncbi.nlm.nih.gov/30566197/
Miller and Prewitt (2012). The Role of State Behavioral Health Agencies in Accelerating the Integration of Behavioral Healthcare and Primary Care to Improve the Health of People with Serious Mental Illness. National Association of State Mental Health Program Directors.
Miller, S.D., Hubble, M.A., Chow, D., & Seidel, J. (2015) Beyond measures and monitoring: Realizing the potential of feedback-informed treatment. Psychotherapy, 52:4, 449-457. https://www.scottdmiller.com/wp-content/uploads/2016/08/Beyond-Measures.pdf
Obisike, E. E. (2018). The effectiveness of telemedicine on stigmatization and treatment burden in patients with health compromising lifestyles and chronic diseases: A critically appraised topic. Open Science Journal, 3(1). https://www.researchgate.net/publication/323549112_The_effectiveness_of_telemedicine_on_stigmatization_and_treatment_burden_in_patients_with_health_compromising_lifestyles_and_chronic_diseases_A_critically_appraised_topic
Rauschenberg C, Schick A, Hirjak D, Seidler A, Paetzold I, Apfelbacher C, Riedel-Heller S, Reininghaus U. Evidence Synthesis of Digital Interventions to Mitigate the Negative Impact of the COVID-19 Pandemic on Public Mental Health: Rapid Meta-review. J Med Internet Res 2021;23(3):e23365. https://www.jmir.org/2021/3/e23365/
Wampold, B.E. (2015). Routine outcome monitoring: Coming of age—With the usual developmental challenges. Psychotherapy, 52:4, 458-462. https://pubmed.ncbi.nlm.nih.gov/26641376/
World Health Organization. (2019). Making the investment case for mental health: a WHO (No. WHO/UHC/CDNCD/19.97). World Health Organization.
Youn, S.J., Kraus, D.R., & Castonguay, L.G. (2012) The treatment outcome package: Facilitating practice and clinically relevant research. Psychotherapy, 49:2, 115-122. https://pubmed.ncbi.nlm.nih.gov/22642519 /